HIV in Canada: A 2025 In-Depth Report
- Home
- HIV in Canada: A 2025 In-Depth Report
HIV in Canada: A 2025 In-Depth Report
By the year 2025 Canada reaches a decisive point in its fight against HIV (Human Immunodeficiency Virus). Medical treatments and public health efforts worldwide have achieved significant improvements yet the number of HIV diagnoses in Canada continues to rise over recent years. Unlike Canada which shows a rising number of HIV cases, new HIV infections continue to fall in multiple high-income nations that are part of the G7 coalition. The consistent rise of HIV infections across Canada has generated alarm among healthcare providers as well as advocacy groups and community leaders who remain heavily invested in transmission reduction programs. The report extensively examines the HIV situation in Canada as of 2025 with recent data analysis alongside assessments of key affected populations, regional disparities and ongoing policy recommendations. Modern statistics and practical observations show that despite increased awareness and better medical treatments saving many lives we still need to continue working towards progress.
Understanding the progression of HIV from its initial outbreak in the early 1980s to modern times provides essential context. During the peak of the HIV outbreak in North America and across the world people died quickly from AIDS after contracting the virus without treatment. The development of antiretroviral therapy (ART) has dramatically transformed the prognosis for HIV-positive individuals because it suppresses viral load levels to enable patients to achieve a near-normal lifespan and achieve almost complete transmission prevention when viral load suppression occurs. Despite advancements in treatment HIV remains incurable and there are still major differences in infection rates and healthcare access. The narrative of HIV in Canada started with men who have sex with men in major cities during the late 20th century but has expanded to affect various groups including women and Indigenous populations. The broader reach of HIV across various populations indicates a requirement for sophisticated responses that integrate harm reduction initiatives and destigmatization along with culturally sensitive healthcare services.
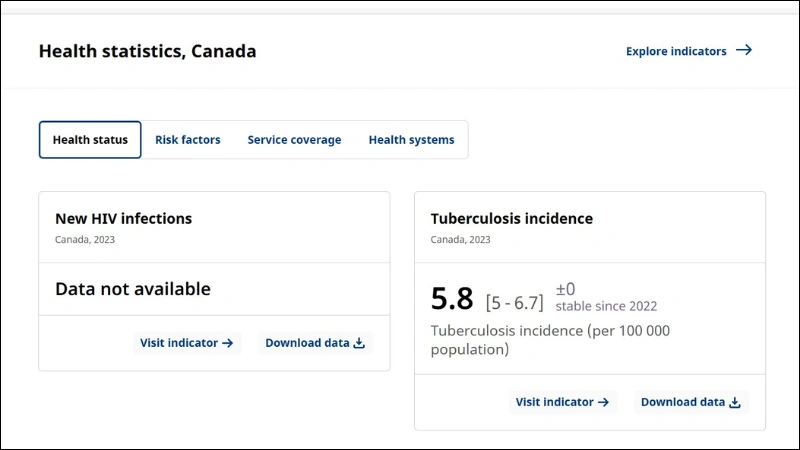
The Public Health Agency of Canada (PHAC) recently reported that 2,434 individuals received new HIV diagnoses in 2023 which shows a 35 percent increase from the previous year. The reported data set the national rate of new HIV diagnoses at 6.1 per 100,000 population demonstrating Canada’s ongoing struggle with rising infection numbers when compared to pre-pandemic statistics. Multiple experts present distinct explanations regarding this increase. The disruption to HIV testing services throughout the COVID-19 pandemic resulted in reduced testing for 2020 and 2021, which led to an artificial reduction in reported case numbers during those periods. The availability of testing increased in late 2021 and 2022 which resulted in statistics rebounding to show newly discovered infections that were not previously reported. The ongoing climb in numbers cannot be explained solely by disruptions in testing activities. Healthcare supporters maintain that regional disparities in harm reduction service access and prevention program funding inconsistencies have intensified current healthcare gaps.
To assess HIV’s scale in Canada, one must analyze both incidence numbers, which show new cases annually, and prevalence, which reflects the total HIV-positive population. Predictions indicate that the number of Canadians living with HIV reached 68,000 by 2024 from 62,800 in 2020. Many people within this group probably do not know their HIV status. Health authorities stress the importance of routine accessible HIV testing since early detection and treatment, beginning with antiretroviral therapy, improve patient health outcomes and prevent disease spread. Canada’s universal healthcare system aims to cover HIV treatment, but a coverage gap, alongside healthcare stigma and socio-economic barriers, often restricts consistent care engagement.
The PHAC surveillance data from 2023 shows a 35 percent rise in new diagnoses, which puts Canada in an unusual position relative to other G7 countries. The majority of nations within this cohort have experienced continual decreases in HIV rates over the last ten years through integrated prevention initiatives and broad implementation of PrEP and PEP alongside strong harm reduction programs. Health advocates throughout Canada acknowledge the significance of current measures but insist those initiatives require expansion and full implementation to serve underserved populations. The Canadian AIDS Society, alongside CANFAR, has called for stronger federal and provincial actions to address HIV prevention in areas where new diagnosis rates are highest. They worry that without continuous financial support and an integrated approach to policy development, the prevalence figures will keep escalating.
The complexity emerges from the notable regional differences in HIV incidence throughout the country. The provinces of Saskatchewan and Manitoba show the highest numbers of new HIV cases, with rates of 19.4 and 19.3 per 100,000 people, respectively. The rates of new diagnoses exceed the national average of 6.1 per 100,000 by a significant margin. The majority of new HIV cases in both provinces stem from injection drug use, which affects urban areas like Saskatoon, Regina, and Winnipeg as well as smaller communities. Prince Albert in Saskatchewan reached an alarming peak infection rate of 56.4 HIV cases for every 100,000 residents at one time. Local organizations in these regions insist that enhanced access to harm reduction services, such as needle distribution and supervised consumption sites, along with educational outreach, remains essential. Adequate support for these programs has led to some progress in stabilizing infection rates or stopping their escalation. The persistent provincial debates regarding the presence and placement of supervised consumption sites generate uncertainty about infection trends because shutdowns or limitations on these facilities can lead to equipment reuse that increases HIV and other blood-borne infection risks.
The majority of provinces and territories experience lower HIV rates, which include British Columbia, along with the Atlantic region and northern Territories, and some report rates below 3 per 100,000. The provinces of Ontario and Quebec, which encompass Toronto and Montreal’s large cities, consistently report infection rates between 5 and 6 per 100,000 even though these dense urban centers experience higher total case numbers. Montreal reports about 12.4 new HIV cases for every 100,000 residents, while Toronto shows approximately 9.6 cases for the same population size. Provincial governments and local health authorities need to create HIV prevention and treatment strategies that meet specific local needs because a universal approach does not work for every context. HIV prevention strategies for Saskatchewan need to address drug use in smaller communities, while Toronto and Montreal require different approaches because men who have sex with men represent most of their new diagnoses.
Although men who have sex with men used to represent the largest HIV-affected group in Canada, historical data shows that current diagnoses are expanding across various populations. For the first time in 2022, heterosexual transmission became the leading route of HIV infection in some provinces, which signals that a lack of proper prevention information and resources can make anyone vulnerable to HIV. The 2023 statistics showed that females accounted for 791 new HIV cases, which equates to a rate of 3.9 instances per 100,000 people. The fact that women can contract HIV from heterosexual sex or injection drug use demonstrates that public health messages need to expand beyond the outdated focus on gay men. Trans women and women who use drugs, along with those from racialized communities, encounter multiple stigmas that often prevent them from accessing essential testing and care services. Studies on HIV transmission during childbirth show that widespread antiretroviral therapy for pregnant people living with HIV significantly reduces the risk of the virus being passed to their babies. HIV transmission occurs infrequently when patients fail to receive appropriate care, which demonstrates the necessity of delivering timely interventions to all population groups.
The use of injection drugs stands as a key element driving HIV transmission rates which peak in certain provinces. People who share equipment for drug injections face a risk of infection from HIV and hepatitis C among other blood-borne diseases. Experts in public health from these regions emphasize the need for needle exchange or needle distribution programs alongside street outreach teams. These interventions deliver sterilized supplies and create access to testing, counseling, addiction services and antiretroviral therapy. Harm reduction outreach programs in northwestern Ontario have managed to stop the growth of previously increasing figures. The effectiveness of local strategies depends on continued financial backing and supportive policies. The elimination or restriction of supervised consumption sites and needle distribution programs leads to an increase in new HIV infections because people revert to unsafe injection habits and lose essential healthcare system links.
Identifying at-risk populations for HIV transmission represents only one facet of the contentious legal debate surrounding HIV disclosure requirements in Canada. The nation maintains strict regulations against HIV status non-disclosure which allow for criminal prosecution when individuals fail to warn partners about potential HIV transmission before sexual contact. After the Department of Justice Canada conducted a review in 2022 legal advisors note minimal progress which continues to cause concern about legal fears deterring HIV testing or treatment access. This situation poses a public health concern: Individuals who fear learning about their health status or sharing it with others tend to transmit the virus without knowing it.
In Canada HIV remains an ongoing challenge because stigma and discrimination act as major obstacles. Decades of public health campaigns have diminished some misconceptions about HIV transmission through casual contact but people still maintain old-fashioned beliefs about the virus. The stigma creates obstacles that stop people from seeking HIV testing and disclosing their status along with accessing healthcare services. Stigma intersects with racism and discrimination against those who use drugs, as well as transphobia and sexism to intensify the challenges faced by people who belong to multiple marginalized groups. Community-based organizations regularly point out how stigma prevents people from receiving proper prevention and care services. Their advocacy focuses on educational programs that spread the message that individuals with an undetectable viral load cannot transmit HIV (the “U=U” or “Undetectable = Untransmittable” concept) and that HIV transmission does not occur through regular social contact.
Advocates regularly recognize supervised consumption sites as crucial components for harm reduction strategies. The facilities provide sterile injecting supplies along with medical supervision for overdose prevention and create accessible entry points to additional healthcare and social services. Thunder Bay, Ontario, faced an HIV outbreak declaration in 2019 because of rising infection rates among people who struggled with housing instability and substance use problems. Public health authorities have praised street outreach programs for linking individuals to testing and HIV treatment, which helps keep the spread of infection under control. Some provincial policymakers are shutting down or imposing restrictions on these sites because they worry about their proximity to schools and other community spaces. Healthcare professionals warn that cutting back on supervised injection sites will lead to increased HIV transmission because drug users might start injecting drugs without supervision and share needles.
The variations in HIV rates across provinces serve as evidence of existing healthcare funding inequalities because they also reveal distinct regional attitudes toward harm reduction. The Canadian AIDS Society, along with other advocates, requested seven-point-two million dollars each year for five years to support community-based organizations and demanded one hundred fifty million dollars in bilateral funding across three years for provincial and territorial assistance. These proposals match Canada’s commitment to eradicate HIV as a public health threat by 2030, following an internationally-agreed-upon timeline. Medical care and prevention backed by strong research activities, together with active community engagement, are essential to accomplish this objective. Antiretroviral therapy turned HIV from an almost certain death sentence in the 1980s into a manageable chronic condition for many people, but research investment remains essential to tackle long-term complications and develop solutions against drug-resistant HIV strains and potential vaccines.
The country’s colonial past, together with its enduring effects on Indigenous peoples, remains an important factor to consider. Indigenous populations experience higher HIV risks because of intergenerational trauma and geographic isolation, along with healthcare settings that lack cultural safety. In Saskatchewan, Indigenous communities experience a much higher rate of new HIV diagnoses compared to other populations. Limited access to culturally relevant health services combined with racialized stigma intensifies these existing challenges. Indigenous-led health programs combat these challenges through their integration of Western medical methods with traditional practices, which results in culturally sensitive and comprehensive care. Participants in health advocacy argue that resolving the HIV crisis in Indigenous populations requires broader reconciliation processes alongside the decolonization of healthcare systems.
People of African or Caribbean heritage, along with Black communities, face significant HIV burdens that surpass their population size in Canada. The available statistics reveal that Black communities and individuals of African or Caribbean heritage show a disproportionately high number of new HIV cases relative to their segment of the overall population, despite incomplete and inconsistent racial and ethnic data collection. A combination of systemic obstacles, like racism, together with economic disparity and immigration-related challenges, acts as a barrier that prevents people from seeking timely HIV testing and treatment. Community organizations respond by implementing outreach programs that include distributing educational resources in multiple languages and collaborating with religious groups to connect with people who would otherwise stay untested because of stigma or isolation. The creation of these initiatives demonstrates how important it is to integrate cultural competence and inclusive practices into HIV prevention and care strategies.
Public information campaigns play a crucial role in the prevention of new infections. Health agencies are now broadening their messaging to communicate that HIV affects all people rather than focusing primarily on gay men. Many young people do not understand how severe HIV and AIDS were in previous decades and thus need education about existing treatments alongside the vital importance of prevention and testing. Low-cost testing drives, alongside at-home test kits and National HIV Testing Day events, work together to eliminate obstacles preventing people from learning their HIV status.
The financial burden associated with HIV prevention and treatment remains significant. Public healthcare plans across all provinces cover basic medical treatments, but access to preventive measures like PrEP remains challenging or costly in specific regions. While some provinces have expanded PrEP coverage successfully, others have not, which results in many people who need PrEP remaining without its support. Experts suggest that expanding PrEP access proves to be financially sound because preventing HIV infection helps avoid the heavy future costs of treating the disease over a lifetime. Individuals benefit from PrEP because it eliminates the emotional, social, and medical issues related to living with HIV.
Canada’s HIV trajectory has been shaped by the lasting effects of the COVID-19 pandemic. The initial lockdown stages of 2020 disrupted several non-critical healthcare operations, which led to interruptions in HIV testing services. The reduction in reported HIV diagnoses during 2020 and 2021 occurred because people did not receive or seek testing during these years (). The reopening of society along with the return to normal operations at testing sites meant that previously undetected cases contributed to the observed spike in new infections. Analysts suggest that actual HIV transmissions increased during pandemic shutdowns because harm reduction services faced restrictions while social isolation and mental health stressors worsened. In 2025 community organizations along with policymakers handle the residual effects from these disruptions which underscores the essential function of dependable public health infrastructure to prevent such challenges.
Several proposals aim to combat the HIV epidemic in Canada. The strategies involve enhanced public education campaigns that inform people about the realities faced by those living with HIV while stressing the need for regular testing and stigma reduction. The proposed plans call for the growth of harm reduction programs in areas where injection drug use persists despite being concealed from mainstream medical services. Data collection improvements on race, ethnicity, gender identity, and sexual orientation enable targeted resource distribution to the areas that need it most. Advocacy groups work tirelessly to reshape Canada’s criminal laws regarding HIV non-disclosure so they reflect modern scientific research about HIV transmission and promote testing instead of penalizing those who receive tests. A healthcare system that integrates HIV prevention and addiction treatment with mental healthcare and primary care services through one coordinated operation would maintain patient engagement while substantially reducing transmission risks.
The future success of Canada in reaching the global goal to eliminate HIV as a public health threat by 2030 remains uncertain. Recent years have shown a significant increase in new diagnoses with 2023 data revealing a substantial spike that underscores the pressing nature of this health challenge. Targeted local strategies have shown success in reducing infection rates or keeping them stable in numerous examples. Healthcare experts stress that ongoing research may yield a vaccine or cure eventually but they do not anticipate these solutions to become available in the near future. Proven methods such as large-scale testing together with immediate treatment and strong harm reduction programs alongside educational outreach continue to be necessary until that time. A country that has established universal healthcare systems presents an opportunity to implement a cohesive national HIV strategy that could reverse current trends in the future.
Effective solutions must address both the virus and the social and economic factors that increase risk across multiple communities. The main factors include a shortage of housing options and systemic discrimination, alongside the absence of healthcare that respects cultural safety and obstacles that prevent people from accessing prevention tools and treatments such as PrEP on time. The HIV numbers in Canada serve as evidence for broader problems of societal inequality and exclusion. Public health experts agree that enhancing HIV prevention and care will also help achieve larger social objectives related to equity and inclusion.
In 2025, Canada reaches an important stage in its longstanding fight against HIV. While treatment and prevention options for HIV have reached unprecedented levels of effectiveness, new infection rates continue to rise for marginalized groups who are racialized or drug users. The fight against HIV requires wider harm reduction programs and integrated HIV prevention within healthcare systems, policy changes to eliminate criminal laws that deter testing and disclosure, as well as stronger public awareness campaigns to eliminate stigma. The objective to eliminate HIV as a public health threat continues to be unattainable without comprehensive and inclusive strategies. If public health agencies and policymakers join forces with community leaders and residents across Canada to implement established interventions, there is still reason to maintain cautious hope. Current data serve as both a warning and a call to action: The direction of HIV in Canada will only shift if all stakeholders maintain continuous dedication while increasing financial support and working together to expand healthcare access and social justice.
References
Public Health Agency of Canada. (2024). HIV in Canada: 2023 surveillance highlights. Government of Canada. https://www.canada.ca/en/public-health/services/publications/diseases-conditions/hiv-2023-surveillance-highlights-infographic.html
CBC News. (2023, September 21). HIV cases rising in Northwestern Ontario, health officials say. CBC News. https://www.cbc.ca/news/canada/thunder-bay/hiv-cases-northwestern-ontario-1.7402508
CATIE. (2024, March 28). How common is HIV in Canada? CATIE—Canada’s source for HIV and hepatitis C information. https://www.catie.ca/essentials/statistics/hiv-statistics?gad_source=1&gclid=CjwKCAjwk43ABhBIEiwAvvMEB04Cd3-o0CWBOmYSNWOrYhryxELSJrEptTXl_uzXoRBKtZwC_ibrwxoCTwwQAvD_BwE
Canadian Foundation for AIDS Research. (2024, February 7). CANFAR unveils “bold strategic” plan to address rise in HIV cases and end the HIV epidemic in Canada by the end of 2025. https://canfar.com/canfar-unveils-bold-strategic-plan-to-address-rise-in-hiv-cases-and-end-the-hiv-epidemic-in-canada-by-the-end-of-2025/
- Share
Magazica
Magazica is a dedicated platform for businesses, subject matter experts, health advocates, and various sectors within the health industry. At Magazica, we are committed to sharing the latest health information and developments with our audience. We serve as a gateway for health-related businesses to showcase their progress and advancements, demonstrating how they contribute to enhancing people's wellness.
